|
Stomach Acid Is Good For You
The
many dangers of acid blocking medications
Terminology:
integrative medicine[i] 5
instances;
translational medicine[ii] 3 instances;
Proton pump inhibitors (PPIs) 36 instances;
Story
at a Glance:
•Many pharmaceuticals on the market are automatically given to large
numbers of patients despite the harms of these medications often greatly
outweighing their benefits.
•One of the worst offenders are the acid suppressing medications, and
their overprescription goes hand in hand with a widespread medical
blindness to the critical functions of hydrochloric acid throughout the
body and the actual causes of acid reflux.
•A variety of safe and non-invasive approaches exist to address the wide
range of (often unrecognized) complications from acid reflux and
dysfunctional stomach acid production.
Note:
this article is a bit on the longer end, but since the stomach acid
issues profoundly affect so many people, I felt I this article needed to
be able to cover all the key points.
One
of the more depressing parts of being an awake physician in
the medical system is reading the drug lists of the patients you see and
realizing how many prescriptions they are on that do not benefit them,
and in many cases harm them. Presently, 66 percent of U.S. adults are estimated to
have at least one prescription and on average, they have 9 prescriptions
filled per year (which can include renewals of an existing one).
Since
doctors are extremely reluctant to terminate existing prescriptions, this
creates a scenario where people get placed on more and more drugs as they
age (some of which are for treating the side effects of other drugs they
are taking).
This situation is even worse for the elderly, who both have more time to
be put on an increasing number of medications and due to their altered
physiology are also the most vulnerable to the harmful effects of those
mediations. For example, from 2009-2016, after 2 billions office
visits were assessed,
it was found that for adults over 65, 65.1% were on two or more drugs, 48.9%
were on four or more, and 36.8% were on more than five (with the highest
use occurring in the oldest Americans).
One
of the best illustrations of the problem came from a study that
compared 119 disabled elderly adults living in nursing homes to 71
matching controls. These patients (who on average were on 7.09
medications) were screened for which of their medications clearly met
the existing criteria for being discontinued (on average 2.8 per
patient). After those medications were discontinued in the test group,
when compared to the controls who remained on all of their existing
prescriptions it was found that:
•The death rate
dropped by 23% (in one year, 45% of the control group died whereas 21% of
the test subjects died).
•The annual rate of
hospital referrals dropped by 18.2% (30% of the controls vs. 11.8% of the
study).
•Not
surprisingly, there were also significant cost savings from withdrawing
the unneeded medications.
In
short, doing nothing except terminating some of the most egregious
prescriptions for our elders (who often lack the autonomy to refuse their
prescriptions) resulted in a 23% reduction in their death rate. When you
consider that many of these drugs are approved for much smaller
reductions of the death rate, and that they frequently have a variety of
other concerning side effects (e.g., triggering dementia), the absurdity of this situation (e.g.,
that this pivotal study never changed how we practice medicine) becomes clear.
For
example, almost everyone is put on statins—especially as they get older,
yet in trials evaluating statins, for instance to evaluate their effect
on 50-75 year old patients’ risk of heart disease, statins caused a 0.4% reduction in
the annual risk of a major cardiovascular event (most of which are not fatal)
and no benefit in the overall death death rate. Likewise, according to
the existing trials (which are almost certainly biased to favor the
pharmaceutical companies funding them), it was found on average that
taking a statin for five years would increase your expected
lifespan by three days. In contrast, statins are notorious
for causing adverse effects which affect at least 20% of recipients.
These effects include cognitive impairment and dementia, personality
changes, loss of sensation throughout the body and significant muscle
weakness or muscle aches.
This
seems absurd until you also consider that statins are also one of the
most profitable drug markets in existence.
Note:
a more detailed summary of the tragic
adverse effects of statins can be found here.
The
Forgotten Side of Medicine is a reader-supported publication. To receive
new posts and support my work, please consider becoming a free or paid
subscriber.
Subscribed
The Worst Drugs on The Market
A
frequent question I receive is what the most harmful medications in
America are. Prior to the COVID-19 vaccines (which I feel have earned
that distinction) there in turn were two ways I interpreted that
question.
1.
Which medications are frequently prescribed to everyone,
often provide minimal benefit, and cause real harms you frequently seen
in practice?
2.
Which medications are highly toxic and have more narrow
uses, but are nonetheless frequently given to patients in many cases
where the harms of doing so far exceed any possible benefit.
In
regards to the first interpretation, almost
every integrative physician I’ve ever asked for their top 5 has listed
the following:
•Proton pump inhibitors (PPIs—the focus of this article)[iii]
•SSRI antidepressants (e.g., Prozac)
•Statins
•NSAIDs (e.g., Ibuprofen)
•Birth control pills.
Note: some have also argued tylenol, benzodiazapines (e.g., valium)
and flu shots also belong on the above list. Likewise, opioids used to
always be on it, but now that the government has gone in the opposite
direction and curtailed their prescribing, so they are no longer widely
distributed and hence no longer can be in the first category.
In regards to the second interpretation, there are
many more answers, but some of the most common ones include:
•Anti-psychotic meditations (used for a wide variety of mood
disorders)
•Accutane (used for acne)
•Ciprofloxacin and other fluoroquinolone antibiotics
•Finasteride (commonly used for hair loss)
•Gadolinium (this is used as a contrast agent for MRIs)
•Gardasil (the HPV vaccine)
•Lupron (which amongst other things is used as a puberty blocker)
In sales, a common practice is to start with a free or low cost item, and
then from the pool of people who get it, use their investment to sell
them a moderately priced item, and then from the pool of those buyers,
sell a more expensive item and so forth. This business practice, in turn,
is known as creating “sales funnels.”
Frequently,
with the above drugs, I see a variety of sales funnels. For
instance, adolescent girls are frequently put onto birth control pills by
their pediatricians (e.g., this survey found
54% of women aged 15-19 had used the pill)—often for reasons unrelated to
sex (e.g., painful periods or PMS in a twelve year old).
Birth
control pills in turn frequently cause significant mood swings and mood
alterations (e.g., a large study detected
a 130% increase in the rates of depression during the first two years of
using the pill), which often leads to these new mood disorders being
“treated” with an SSRI antidepressant (which now more than 10% of teenage
girls are on). In turn, one of the more common side effects of SSRIs are
other new psychiatric disorders (bipolar I is the most common) which are
then treated with an antipsychotic (or another mood stabilizer).
As a result, I often meet young women who went through this sales funnel
in their adolescent years and now are on the fairly damaging
anti-psychotics. Additionally, I’ve also spoken to a few people who had
been on this pipeline and said the neuropsychiatric damage they developed
from the HPV vaccine was ultimately tipped them over the edge (which then
required taking an antipsychotic which frequently caused even more
chronic psychiatric and neurological issues for them).
As
you might guess, I am not a fan of this business model, and one of my goals here is to gradually go through
why each of these drugs cause so many problems.
Translational Medicine
Since
medicine is supposed to be “science based,” a
recurring question is why the most important scientific discoveries are
never adopted into clinical practice, or if they are, often take years if
not decades to be (this is what the discipline of translational medicine
seeks to address). This for instance has been shown with the
COVID-19 vaccines, as over and over, the evidence demonstrated they were
neither safe nor effective, but nonetheless every clinical guideline
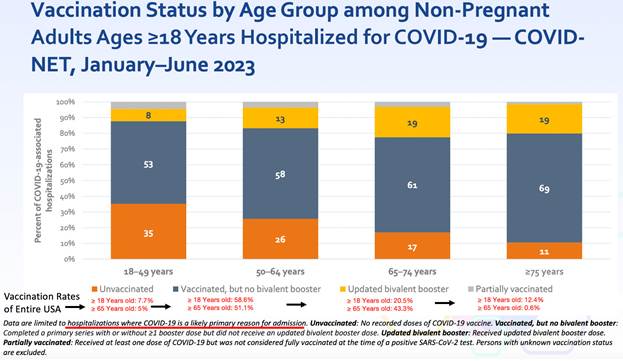
keeps on recommending their use on everyone. For instance, consider how
effective the vaccines are per the CDC’s own recent admission:
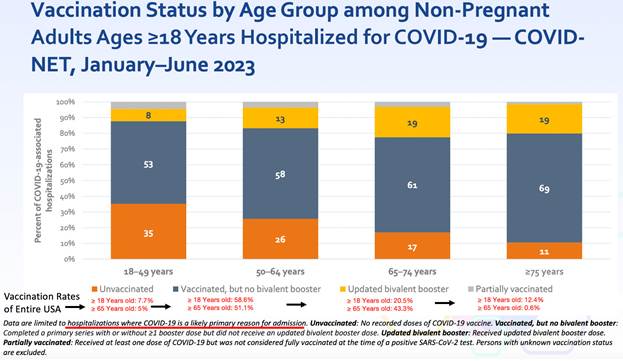 Note:
the population vaccination percentages were sourced from this CDC dataset,
which I believe likely overestimates how many people were vaccinated, as
at least 25% of the people I know never received the vaccine, whereas the
CDC claims only 7.7% didn’t. Note:
the population vaccination percentages were sourced from this CDC dataset,
which I believe likely overestimates how many people were vaccinated, as
at least 25% of the people I know never received the vaccine, whereas the
CDC claims only 7.7% didn’t.
If
you look at the above data, it’s clear this vaccine is not an effective
product, and once the harms of the vaccine are also taken into
consideration, especially given how vocally opposed the public is to
those products, it becomes very difficult to justify continuing to use
them. Nonetheless, the FDA is still rubber stamping the newest COVID
vaccines (with virtually no data to base the approval upon) and hospital systems are
beginning to mandate the new booster for their employees.
I believe all of this helps to illustrate how resistant the medical field
is to acknowledging data which challenges existing beliefs.
Note: I always believed the COVID-19 business model was to saturate
one market at a time and then pivot to the next one once the previous was
saturated. This for example is why we saw a successively more aggressive
series of pushes to sell the vaccines (e.g., first selling them through a
scarcity model, then with financial incentives, then soft mandates, and
then eventually hard mandates) or why the vaccines were pushed onto
children (who have no risk of dying for COVID-19) once adults no longer
were willing to receive more of the vaccines. Likewise, I previously
argued that once no more of the initial two-shot series could be sold
that they would pivot to acknowledging it didn’t work (e.g., see this recent announcement by
the governor of New York) so that the boosters which “did work” could
next be sold to the public.
When
I first started my medical education, a mentor told me:
The
medical profession has always been remarkably conservative in adopting
new ideas. Try not to get frustrated if they won’t consider the evidence
you present to them.
In
turn, on this Substack, I’ve tried to gradually review examples of the
widespread refusal of the medical profession to consider critically
important evidence that was being presented to them. By doing so, I’ve
hoped to show how this behavior is the norm rather than the exception, so
each of you better understand why there has been such a steadfast
rejection of the science throughout the pandemic.
For
example, I am a long time fan of Dr. Mercola (I’ve read his website for
decades). A major reason I’ve read it has been because Mercola has
repeatedly presented ideas (with compelling science to support them)
about medicine and health the medical community rejected, and over and
over I’ve seen those ideas be accepted as self-evident truths years later
by my profession (e.g., Dr. Mercola corrected [correctly] predicted
that Vioxx would be a disaster).
The reason I mention all of this is because despite Mercola having the
most read natural health website in the world (leading to many patients
demanding what he puts forward and many physicians adopting his advice),
alongside Mercola’s ability to clearly prove his ideas with existing
science, the medical profession still has
taken years if not decades to accept those ideas. Mercola’s example hence
serves to illustrate just how powerful the barriers to translational
medicine are.
Another
pioneer in the integrative medicine field is Jonathan Wright MD,
and much of the initial knowledge base of integrative medicine came from
his pioneering work, particularly his research (he had a knack for
digging up forgotten research that was extremely relevant to patient
care). In this article I plan to review many ideas I was initially
exposed to by Wright, and many parts of this article (e.g., the
quotations) are summaries sourced from Why Stomach Acid Is Good For
You, a book that was written in 2001. Like Mercola,
many of the ideas Wright put forward with the evidence to substantiate
them were largely ignored by the medical profession—and much of what he
proved about acid blocking medications over twenty years ago is only now
starting to become accepted.
Acid Reflux
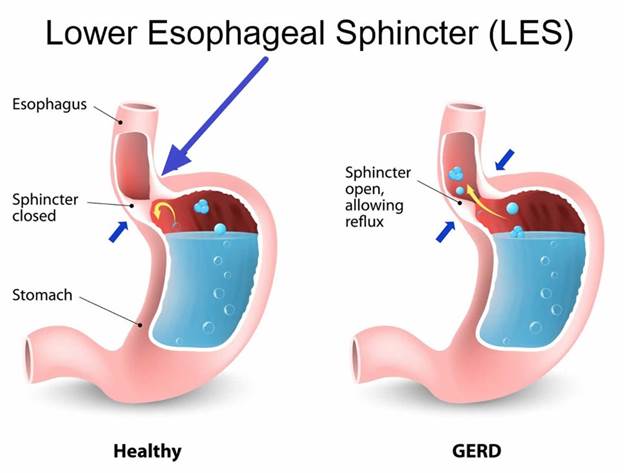
Your
stomach contains acid it uses to digest food (primarily by turning on
powerful enzymes which digest protein). When the stomach is digesting
food, the acid should stay inside the stomach, but sometimes it instead
leaks back up into the esophagus (your throat) because the muscle that
seals the top of the stomach fails to fully seal. Since stomach acid is
irritating, when it refluxes into the throat, it frequently creates the
irritating condition known as heartburn.
Gastroesophageal
reflux disease (GERD) is a very common condition, estimated to affect 20%
of adults (ranging between 18.1% to 27.8% of adults in the USA), is
slightly more common in women, and those numbers have been
gradually increasing globally. Since the heartburn it
typically triggers causes immediate discomfort, people with GERD
typically want it to be treated, especially once their doctor encourages
this (e.g., because otherwise your esophagus can get damaged and potentially turn
cancerous).
In
addition to overt acid reflux, another condition also exists, known as
silent reflux (or laryngopharyngeal reflux), where more minor reflux
occurs without causing overt heartburn. Although I believe medicine tends
to overhype diseases so more medications can be sold for them, I feel
silent reflux belongs to the other camp, as it is frequently not
recognized as the root cause of a variety of other symptoms such as:
•Allergies
•Asthma and reactive airway diseases
•Burning in the mouth or on the tongue
•Chronic sore throat
•Ear pressure and ear infections
•Frequently feeling like you need to clear your throat (and sometimes
cough)
•Post-nasal drip
•Sensation of a painless lump in the throat
•Sinus issues
The speciality of otolaryngology (ears nose and throat [ENT] medicine)
best illustrates the impact of silent reflux as a surprisingly high
number of the issues patients see an ENT for are actually just due to
silent reflux. In turn, better ENTs can recognize and fix those symptoms
by focusing on the silent reflux rather than trying to treat the symptoms
with medications directed at each individual issue. More importantly,
silent reflux tends to have a greater response to lifestyle changes
(e.g., eating different foods) and thus can often be easily treated
without medications (although a brief course of medication is often used
to help a patient recognize that silent reflux is causing their issues).
Stomach Acid Is Good For You
One
of the things I always marvel at is how subtle distortions tend to occur
in science which lead to everyone having a false conception of reality
that conveniently allows a profitably industry to
exist. One such example can be found with stomach acid, something the
medical field views as largely unnecessary and thus possible to justify
eliminating with acid suppressing medications.
Stomach acid for context, serves a variety of critical functions. They
include:
•Making it possible to fully break down protein.
•Sterilizing the stomach so foreign bacteria, viruses, yeasts and
parasites cannot make it into the digestive tract.
•Chelating minerals from food so they can be absorbed.
•Making it possible to absorb certain vitamins and nutrients (e.g.,
vitamin B-12).
•Regulating the rest of digestion.
Yet,
most of these are glossed over. For instance, medical students are taught
to believe protein digestion occurs primarily within the small intestine.
This largely comes about because the the critical functions of stomach
besides digesting protein aren’t typically focused on, and for that
function, doctors in training are taught that the digestive enzymes from
the pancreas are sufficient to digest protein once it reaches the small
intestine, thereby eliminating any need for the stomach’s acid. Within
this paradigm, it thus becomes justifiable to suppress stomach acid as
much as possible with acid blocking medications.
Let’s
now look at why these functions are in fact vitally important.
Note:
typically with medical interventions and correlated conditions, you see
small to moderate correlations between them. One of the most striking
things about stomach acid is over and over again how large the effect of
adequate vs. inadequate stomach acid is—in most of the studies Wright
cited that we will discuss in the following sections, between a two to
ten fold difference could be observed once sufficient stomach acid was
present.
Protein Digestion:
Proteins
are composed of long chains of amino acids which then fold into a variety
of complex structures which create our cellular infrastructure. To digest
proteins, those chains must be broken apart and then disassembled into
their constituent amino acids (which are then assembled back into
proteins within the body). If this does not happen, the body becomes
unable to extract the amino acids it needs from the proteins you eat,
which in turn causes significant nutritional deficiencies.
Amino acid deficiency is a widespread problem, and in both my practice
and that of my colleagues, we frequently find one of the most important
supplements for our patients is the correct mix of predigested amino
acids. Likewise, it’s frequently observed that amino acid deficiencies
are linked to psychiatric conditions because some of the amino acids form
the building blocks of the neurotransmitters which regulate your mood. As
a result, supplementing with amino acids is often a critical component of
an integrative psychiatry plan (e.g when assisting a patient with
withdrawing from a SSRI antidepressant—which are notorious for being
highly addictive and difficult to quit).
When
proteins are not digested, their fragments are often able to pass from
the gut into the bloodstream where they trigger a wide range of food
sensitivities. In turn, I frequently find that with patients who have a
wide range of food sensitivities (which requires them to eat very
restrictive diets), their issue is poor protein digestion rather than a
specific a food allergy. More importantly (and a key reason why I wrote
this article) was Wright’s observation that a wide range of autoimmune
conditions are directly linked to low stomach acid levels.
Note:
food allergy tests are fairly inaccurate and yield highly variable
results (e.g., colleagues have found that two samples taken at the same
time from the same patient but sent in under different patient names
yielded significantly different results). I am not sure if this issue has
been improved in recent years since we stopped using those tests and thus
can no longer evaluate them.
Sterilizing the Stomach:
A
key function of stomach acid is to sterilize the GI tract so that
microbes cannot enter and colonize it (as the GI tract otherwise
represents an ideal area for them to inhabit).
The importance of the sterilization is the most apparent with acute
infections. For example, individuals on acid suppressing medications have
a much higher risk for developing food poisoning after eating a food
infected with one of many bacterial species known for that (individuals on
acid suppressing medications have been found to be around 4 times as
likely to develop one of these
infections).
Likewise,
for centuries, it was well known that cholera (an infections that was a
scourge to humanity until we cleaned up our water supply) was
dramatically more likely to affect those with deficient stomach acid. For
example, in 1885, Robert Koch (who discovered many of the fundamental
characteristics of microbial infections) found that feeding guinea pigs a
dose of bicarbonate (an antacid) before infecting them with cholera
dramatically increased their risk of developing the infection. Likewise,
in numerous cholera outbreaks, public health officials have found those
who developed infections had low stomach acid levels, while those who did
not had normal levels.
While
cholera is now largely a thing of the past, the area where this acute infection
risk is the most significant is in hospitalized patients who are
routinely put on acid suppressing medications (especially if they are on
ventilators). A variety of studies have shown those put on acid
suppressing medications are more likely to catch those (sometimes fatal)
hospital acquired infections.
For
example, one study in the New England
Journal of Medicine found that ventilated patients
who received an acid blocking medication (which was not as powerful as
the newer PPIs) were twice as likely to develop pneumonia and 60 percent
more likely to die from hospital acquired pneumonia. Similarly, a
Clostridium difficile infection is the leading cause of
hospital-associated infectious diarrhea and has considerable impact on
the length of a hospital stay and its costs—those on PPIs were
found to be twice as likely to
develop this condition. Furthermore, one large review of
septic patients found those on PPIs were 4.3% more likely to die than
those not on PPIs.
Note: the largest review that
has been done so far of PPIs and COVID-19 found PPIs increased a COVID
patient’s risk of dying by 77%.
Many
of the issues with acid suppression are best illustrated by how they
alter the normal bacterial flora of the gut. For example, to quote the manufacturer of
one PPI:
As
do other agents that elevate intragastric pH, omeprazole [Prilosec]
administered for 14 days in healthy subjects produced a significant
increase in the intragastric concentrations of viable bacteria. The pattern
of the bacterial species was unchanged from that commonly found in
saliva. All changes resolved within three days of stopping treatment.
While
bacterial colonization in the stomach is potentially problematic, it is
much more of an issue as those microbes are able to travel further into
GI tract. For decades, the functional medicine community has observed
that inappropriate colonization of the GI tract leads to a variety of
problems, such as the complex and debilitating condition SIBO (small intestinal bowel
overgrowth). Likewise, many others have linked the
inflammatory endotoxins produced by bacteria within the digestive tract
to a wide range of chronic health conditions.
Note:
individuals with significant bacterial overgrowth in the stomach often
report having a horrible breath odor (which is sometimes why they seek
out treatment).
Nutrient Absorption
Many
(myself included) believe one of the primary causes of all the chronic
illnesses we see today are widespread deficiencies of vital nutrients. In
turn, a good case can be made that this deficiency comes from any of the
following:
•Intensive chemical based farming has caused our soils to become
demineralized, leading to plants no longer having the nutrients we need.
Given the dramatic health benefits that have been repeatedly
observed from remineralizing the soil, I feel this is a
very valid concern.
•Chemicals
in the environment block our absorption of essential nutrients. For
example, the widely used herbicide Roundup also happens to be a chelating
agent which is well known for binding to essential minerals (e.g.,
manganese) and preventing them from entering the body.
•The
highly processed food diets we eat do not have many of the essential
nutrients we need (e.g., fat soluble vitamins from animal fats and
organs). Weston Price’s seminal
research best demonstrated the importance of this, as
he repeatedly observed societies that transitioned from their traditional
diet to the modern processed one went on develop the wide range of
degenerative conditions associated with modern life. Likewise, I have
repeatedly seen patients develop significant improvement in their health
once these nutritional deficiencies are addressed.
•Nutritional
absorption is impaired. While this can come from a variety of issues
(e.g., dysfunctional neurological regulation of the GI tract), one of the
most consequential causes is deficient stomach acid.
For
many essential minerals, (e.g., zinc, magnesium, calcium, and iron), acid
is necessary for their absorption as they require an acid environment to
separate into water soluble ions that can enter the body (e.g., iron
absorbs much better at a pH below 5). In one study, it was found antacids
reduce the absorption of iron by between 28-67%, while in another study,
when stomach acid deficient patients (having a gastric pH was 6.5) had
their stomach acid pH lowered to 1 (making it much more acidic), calcium
absorption rose five-fold to 10 percent. Similar differences are also
seen with other minerals.
These
issues are particularly true for minerals bound to plants when compared
to the much more absorbable forms they exist as within animal tissue
(which Wright illustrated with the data on iron absorption—something that
may help to explain some of the fatigue and anemia seen in vegetarians).
Likewise,
many essential vitamins also require stomach acid for their absorption
(e.g., because acid separates vitamins from the protein they are bound
to), with B12 being the best example. There is also significant data
linking B6 and folate absorption to stomach acidity, and some data linking,
vitamin A, B1, B2, B3 and E to stomach acid levels. Most importantly, Dr.
Wright has observed improvement in the absorption of nearly every
nutrient when poor stomach function is improved.
Note: a wide variety of chronic issues (e.g., excessive fatigue,
reduced ability to concentrate, tiredness, insomnia and lack of interest
in the external environment have been linked to B12 deficiencies).
Typically Wright found in patients with chronically impaired gastric
function (which was creating a variety of other illnesses), B12 often
needed to be injected rather than taken orally, but in less severe cases,
oral supplementation alongside supporting gastric function often was
sufficient to address the problem. Additionally, he found in these
patients women had the greatest response to B12.
One
area Wright specialized in treating was macular degeneration. A core (but
not the only) component of his approach was addressing nutritional
deficiencies (which were often due to poor gastric function). To
corroborate this argument, he cited a large study of
the risk factors for macular degeneration:
It
appears that one of the most important risk factors for a subgroup of
individuals with “dry” macular degeneration (those characterized by
“geographic atrophy”) is the use of antacids”
I
agree with Wright’s perspective, especially since my colleague who worked
with him (and held Wright in high esteem) repeated observed Wright’s
success is treating macular degeneration. My only difference of opinion
is that poor blood flow to the eyes (and lymphatic drainage from them)
also plays a critical role in macular degeneration as I have also seen
practitioners who only addressed that part of the picture (e.g., through restoring zeta
potential) also successfully treat macular degeneration.
Digestive Signaling
Many
of the signals that facilitate digestion (e.g., the hormones secretin and cholecystokinin)
are generated by the acidity of the stomach. For example, the pancreas
requires those signals to release the enzymes it uses to digest proteins,
once again making it very frustrating that the much of the medical profession does not believe stomach acid is
necessary for protein digestion. The
important thing to understand is that many of these essential digestive
functions can only occur within a very narrow pH range (which shifts
for each stage of digestion).
Common
signs of this process being impaired include indigestion or flatulence
beginning an hour or more after meals and floating stools. Additionally,
the pancreatic enzymatic function necessary for digestion is often
observed to worsen with age and in diabetes (a disease characterized by
impairment of the pancreas’s other primary function—secreting insulin).
As
the above points show, stomach acid serves many critical functions.
To quote Wright:
“Why
would Nature expend so much metabolic energy to provide each one of us at
birth (and until at least age forty) with an ample supply of stomach acid
and pepsin if it weren’t really necessary for digestion?”
Conditions Linked to Impaired Stomach Acidity
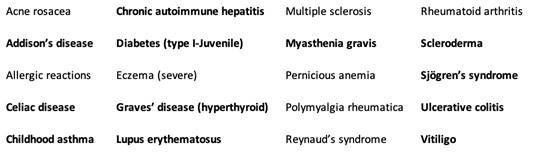
Wright
placed such a heavy emphasis on treating deficient stomach acid because
he found it was such a common thread in the patients he saw, particularly
those with autoimmune conditions—which subsequently improved once stomach
acid function, digestive enzyme function, and the existing nutritional
deficiencies were addressed.
Many
of the conditions he observed matched those which have been linked to
silent reflux—which essentially means silent reflux is always an
important condition to consider even if ears, nose and throat symptoms
are not present. However, in addition to asthma (which can potentially be
explained by refluxing stomach acid or pathologic bacteria which have
colonized the stomach irritating the lungs) many other autoimmune
disorders Wright treated also had a strong link to stomach acid
deficiency, and for many of those disorders, he provided a strong case to
support that link.
For example, in 1931, Dr. Bray published his
discoveries from many years of following more than
200 children with asthma. He found that over 80% of the asthmatic
children had below normal acid secretion in their stomachs, with a mild
deficiency being present in 23% of the children, a severe deficiency
being present in 48% and a complete deficiency existing in 9%.
In most cases, if he provided them with a dilute solution of hydrochloric
acid to drink, in three months their asthma went away, with the
improvement being much faster (and less likely to recur in the
future—particularly over the winter) if allergens were taken out of their
diet. Furthermore, he found for many children, the deficiency was the
most pronounced when they were under seven years of age, and that as they
grew older, many children’s stomach acid secretion returned to normal,
which often coincided with the remission, or “spontaneous cure,” of their
asthma.
Sadder still, Bray was not the only one to find this. Medical literature
on the link goes back as far as 300 years ago and there was a wealth of
data in the 1920s, 1930s and 1940s substantiating it. Unfortunately once
“treatments” such as bronchodilators and steroids were found for asthma
(which could be used for life) all incentives to explore the actual
causes of asthma disappeared).
Fortunately, Wright was incentivized to use these forgotten approaches
and reported:
In
hundreds of cases, I have found that more than 50 percent of children who
come to me with asthma can have their wheezing cured simply by
normalizing their stomach acid and properly administering vitamin B12,
with no bronchodilators and no corticosteroids. I can only give you
approximations, but about 50 percent completely eliminate their wheezing,
about 30 percent have major improvement, about 10 percent only minor
improvement, and only about 10 percent no change.
Note:
Wright also found acid suppressing medications provided minimal
improvement for asthma.
In
total, Wright was able to draw a clear link between stomach acid
deficiency and the following autoimmune conditions (as data existed to
support the link and in over half of the cases he saw, low stomach acid
was detected):
|
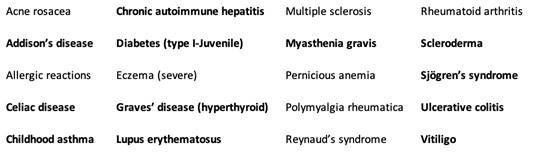
|
|
In
the above list, those conditions in bold are known to be linked to an HLA genetic factor.
However, despite that link, the conditions still responded to treatment,
supporting the argument that many
diseases we view as being genetically inevitable are in fact only
representative of an increased susceptibility to the condition which can
then be treated through addressing the underlying environmental factors.
This is very similar to the situation
with autism, where many different genetic factors have been
partially linked to it, and all of those factors share the common thread
of increasing the likelihood an environmental toxin will permanently
damage the body (e.g., because its ability to detoxify is
reduced, because the body has an increased
sensitivity to entering the cell danger
response, or because the body has a decreased ability to
maintain its physiologic zeta potential). Thus in both
cases, we have a myriad of conditions that are difficult to explain
unless they are each viewed as the manifestation of a few key pathologic
processes.
In
addition to these autoimmune disorders (which Wright typically treated by
restoring gastric acidity, replacing the lost nutrients and avoiding
foods the patient had a sensitivity too), he observed a variety of other
conditions were also frequently triggered by low acidity. These included:
•A
variety of GI related issues (e.g., bloating, poor digestion, poor
absorption of nutrients, SIBO, and of course GERD).
•Skin diseases, including forms of acne, dermatitis (itching, redness,
swelling), dermatitis herpetiformis, eczema, and urticaria (hives)—many
of which are technically autoimmune disorders.
•Accelerated aging
•Depression
•Gallbladder disease (gallstones)
•Hay fever (which is also allergic in nature).
•Macular degeneration
•Migraine headaches
•Osteoporosis
•Stomach
cancer
Note: In his 2001 book, Wright predicted the PPIs would significantly
increase stomach cancer, since as early as 1879 the condition had been
linked to low stomach acid conditions (possibly as a result of allowing
an H.Pylori infection to become more damaging). Recent studies have
confirmed this prediction, typically finding PPIs roughly double the rate
of stomach cancer (e.g., a meta-analysis reviewing
millions of people found PPIs increased it by 1.8 times).
What Causes Acid Reflux?
So
far, I’ve tried to make the case that acid reflux is tied to a stomach
acid deficiency (something Wright found in over 90% of the thousands of
tests his clinic performed), and more importantly, that the presence of
reflux should serve as a warning other parts of your health may also be
compromised due to the possibility a stomach acid deficiency is present.
Sadly, doctors always assume there is too much acid in the stomach when
seeing a patient with GERD rather than measuring the stomach acid levels
prior to beginning an acid reducing regimen (e.g., in 30 years of
practice, Wright never saw a patient, regardless of how many tests they
had to evaluate their GI tract who ever had the acid within their stomach
measured).
All
of this comes about because of an important fact that is never taught in
medical school. The lower esophageal sphincter is pH sensitive and only
closes once sufficient acidity is present in the stomach (which makes
sense since otherwise food would not be able to get to the stomach in the
first place, but once it’s there, you need a way to keep it from getting
back into the throat).
Since GERD is so common, that suggest there is also a widespread
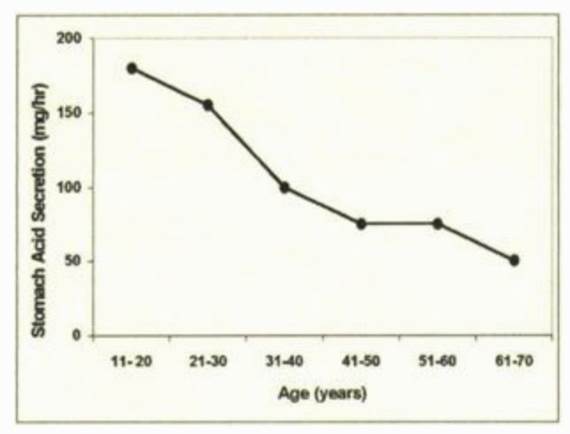
deficiency in stomach (hydrochloric) acid. Presently, I believe a few
factors are responsible that:
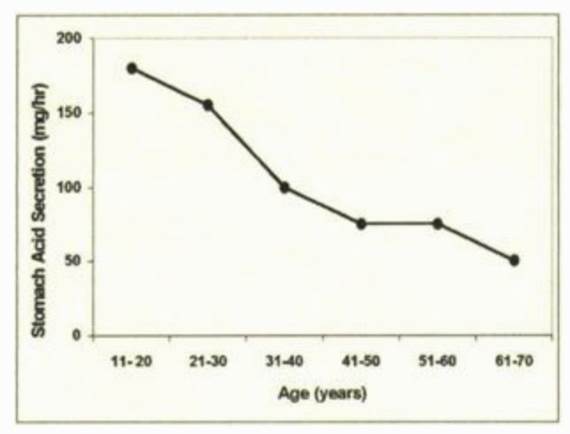
•The first is that stomach acid production is known to decrease as we age
(particularly after 60), and at this time, I consider it to be one of the
primary causes of the degeneration seen in aging and why amino acid and
B-12 supplementation is often so critical for older patients.
|
|
|
Note:
The likelihood of GERD is known to increase with age, which again makes
it remarkable so few doctors consider the possibility excess acid in the
stomach is not the cause of their patient’s symptoms or think to ask (to
quote Dr. Wright): “Why is too much acid so efficient at refluxing back into
the esophagus but so inefficient at actually digesting food?”
•Second,
stomach acid requires both hydrogen and chloride to be produced, and many
of the dietary factors which created each (e.g., sodium chloride) are
much less present in our diet now. In turn, colleagues have found
correctly supplementing these elements often significantly improves GI
function.
•Third,
autoimmune conditions can attack the acid producing cells of the stomach.
•Fourth, H. Pylori infections will decrease stomach acid production.
•Fifth, stomach acid production is an energy intensive process (hence the
cells which make stomach acid having a large number of
mitochondria), and I have long suspected that
mitochondrial dysfunction (something often also seen with many of the
chronic illnesses Wright listed above).
•Finally,
taking acid suppressing medications, does of course reduce the presence
of stomach acid.
However,
at the same time, a stomach acid deficiency is not the only thing which
can cause reflux. It can also frequently occur if too much pressure is on
the stomach (e.g., from a hiatal hernia—a condition estimated to
affect 55%-60% of individuals over the age of 50), thereby popping
the lower esophageal sphincter (LES) open. Likewise, many medications,
particularly ones used to relax muscles like the bronchodilators used
to “treat” asthma, certain blood pressure
medications (e.g, calcium channel blockers)
along with valium, nitroglycerine,
and opioids relax
the LES and thereby allow stomach contents to leak through it.
Additional, Wright found that some foods, including fats, chocolate,
coffee, other caffeinated beverages, mints (especially peppermint and
spearmint), sugar, onions, and some alcoholic beverages, can weaken the
LES.
Finally,
if a substance irritates the stomach, that will frequently trigger reflux
to occur. Some of the most common triggers include acidic citrus fruits
and tomato-based foods, spicy foods, carbonated beverages, and coffee.
Additionally, for patients with lectin sensitivities, the high lectin foods are
often important to avoid.
It should also be noted that a food irritating the stomach is not always
bad. For example, spicy or bitter foods trigger stomach acid
secretion, and in many parts of India, incredibly spicy
foods are the standard cuisine—something many of my colleagues have
suspected emerged in the culture because it protects the natives from the
high number of parasites there (as the stomach acid kills them). However,
while spicy foods (specifically the active ingredient capsicum) trigger
acid secretion and have a protective effect on the stomach’s lining, they
will also irritate already inflamed tissue and hence should not be used
in more severe cases of GERD.
Note:
the foods listed above are typically seen on lists of foods to avoid if
you have GERD, but Wright is the only person I know who broke them into
foods that weakened the LES versus foods that irritated the stomach.
The Problems with PPIs
Presently,
it is estimated that over 27% of Americans take antacids, and that over 15% of
the USA population (increasing with age) take PPIs. For context, PPIs are
the most powerful acid suppressing medications—a single pill often
removes almost all of the stomach’s acid for the rest of the day—but
simultaneously are sold over the counter allowing many to self-medicate
with them.
Note:
some antacids (PPIs and H2 antagonists) work by suppressing the stomach’s
acid production. Others (e.g., Tums) work by directly neutralizing acid
within the stomach. Although the neutralizing ones are the least harmful
(since they have the weakest effect on stomach acid production), many of
those neutralizers contain aluminum hydroxide (a toxic compound which severely impairs
physiologic zeta potential and is frequently added to
vaccines as an adjuvant). Because of this, it is important
to review the ingredients of antacids before you ingest them.
From
reading this article so far, you can likely guess what many of the harms
from PPIs are, and when they were first
approved by the FDA, many of those harms were recognized. As a result,
PPIs were intended to only be used for rare conditions (e.g., Zollinger–Ellison syndrome)
characterized by very high stomach acid levels or in the presence of
significant damage to GI tissue, and if used, to only be used for a 4-8
week period.
Since there was so much money to be made in using PPIs, we instead saw
patients use them for much more common issues (e.g., heartburn) and often
for the rest of their lives. Furthermore, since GERD is often due
to too little stomach acid preventing the LES from closing, once a PPI is
stopped and a bit of the stomach acid returns, rebound GERD often immediately occurs before a normal
stomach acid level is reached and the LES closes on its own. As a
result, after a prolonged period of use, PPIs are often extremely
difficult to quit (e.g., consider that there have been reports of
patients who produced no HCl for two years after stopping Prilosec, a
common PPI that you can now buy over the counter).
Note: a medication which demonstrated short term benefit becoming
problematic when it instead was used for a prolonged period is a
recurring issue in medicine. One of the best examples are the
benzodiazepines (like valium) used for anxiety. These drugs can be very
helpful when used for brief periods of intense stress, but become extremely detrimental and addictive once
they are used indefinitely, leading to many patients becoming chronic
users of the drugs. Two of the other drugs classes that are the most
notorious for creating a lifelong addiction due to their severe
withdrawals are SSRI antidepressants and
opioids.
Likewise,
now that the PPIs are off patient, research
has at last begun to emerge that has corroborated many of Wright’s
predictions about PPIs from thirty years ago. For example in
addition to the harms listed previously (e.g., impaired nutrient
absorption or an 80% increase in stomach
cancer), PPI use has now been linked to:
•A higher risk of dying (e.g., this study found
PPIs increased the overall risk of death by 19%).
•A higher risk of a major cardiac event (e.g., this meta-analysis found
a 28% increase)
•Kidney disease (e.g., this study found
a 74% increase in severe kidney disease, resulting in a 142% increased
risk of death).
•Liver disease and a significant worsening
of existing liver disease.
•Osteoporosis and fractures
•Infections such as the previously mentioned Clostridium difficile
colitis. For example, this study found
a 37% increased risk of community acquired pneumonia in PPI users.
•Hypomagnesemia (low
magnesium levels).
•Dementia (e.g., this recent study found
a 33% increase).
The Forgotten Side of Medicine is a
reader-supported publication. To receive new posts and support my work,
please consider becoming a free or paid subscriber.
Subscribed
Managing Stomach Acidity
Most
of the existing approaches for treating GERD (excluding those which
use acid suppressing medications) and the conditions relating to
deficient stomach acidity normally seek to do one or more of the
following:
•Reduce the pressure on the stomach.
•Remove irritating foods from the diet.
•Restore the tone of the LES.
•Restore hydrochloric acid production.
•Restore damaged areas of the GI tract (e.g., an ulcer) without using
acid suppressing medications.
•Support normal digestive function in tandem with increasing stomach
acidity.
Some
of these approaches are relatively straightforward and have been
mentioned throughout the article. Others are commonly done within
medicine (e.g., a fundoplication wraps
the top part of the stomach around the esophagus thereby tightening the
LES and reducing how much acid can exit back into the esophagus—but
unfortunately has a variety of side effects).
Many
of the effective approaches I and colleagues have used to address GERD
and the complications of low stomach acid are much safer
than a fundoplication. Unfortunately, there
are still precautions with using them, and I ask you to consider
everything in the final part of the article (and ideally find a
physician to work with) before attempting any of it.
Increasing Stomach Acid:
In
the old days, people would drink dilute hydrochloric acid (which
surprisingly worked for a remarkable number of conditions including
lymphatic stasis, tuberculosis and cancer—read this remarkable 1869 book if
you ever have the chance). Not surprisingly, drinking dilute hydrochloric
acid (HCl) was also the mainstay way to treat low stomach acidity.
Note: many people on here ask me about chlorine dioxide. My colleagues
have observed that chlorine dioxide produced with hydrochloric acid tends
to perform much better than that produced with citric acid, which has led
many of us to suspect part of the benefit is from the hydrochloric acid
itself.
However, it is often difficult to obtain HCl, as in high concentrations
it is very dangerous, and oftentimes, patients who try to drink HCl
safely nonetheless injure themselves. For this reason, Wright and now
almost everyone else advises eating a pill HCl is bound to which it then
disassociates from once in the stomach. This is primarily done with
betaine, and as a result betaine HCl is a supplement you can typically
find in the health food store. Glutamic acid is also used, but betaine is
preferred as more HCl molecules can be attached to betaine (although
sometimes patients are sensitive to one HCl carrier and require the other
and as a result some of Wright’s patients were on the Glutamic acid preparation).
A variety of different protocols exist for HCl dosin. Wright for example
suggested:
To
minimize side effects, it is always best to start with one capsule of
betaine HCl containing about 650 mg, with pepsin, in the early part of
each meal. If there are no problems after two or three days, I recommend
increasing the dose to two capsules in the early part of each meal; then
after another two to three days, increase it again to three capsules. We
increase the dose gradually in this stepwise fashion until the
recommended dose (five to seven capsules for the “average”
adult) is reached. When people have to take several capsules with a meal,
I suggest taking half just after the first few bites and half midway
through the meal.
Others
suggest taking as many as you need to get the slightest burning sensation
and then decreasing by one capsule. The exact dose varies greatly person
to person and often depending upon the meal, but almost everyone agrees
HCl pills should be taken with every meal.
In
some cases, individuals cannot tolerate the HCl pills, and instead need
to use a lighter acid, for which lemon juice or apple cider vinegar is
typically preferred.
Note: apple cider vinegar is often extremely helpful for reflux and
colleagues I trust believe it is also an excellent source of the hydrogen
the body needs to make HCl.
Wright
sincerely believed that two things needed to be established before
starting HCl supplementation:
First
that there was indeed a stomach acid deficiency (which was true most of
the time—but not always). Unfortunately, the pills used to test this
(which were essentially a pH meter and a radio transmitter) to the best
of my knowledge are no longer available.
Second,
you needed to ensure there was not pre-existing damage to the stomach (e.g.,
an ulcer), which is frequently caused by the usage of NSAIDs such as
Ibuprofen, along with corticosteroids and aspirin (at a typical dose).
NSAIDs for example are amongst the most commonly used drugs, often cause
damage to the lining of the stomach (and amongst other things kill
thousands of Americans each year from fatal GI bleeds). In these
patients, Wright used a different protocol which involved a lighter acid
(e.g., vinegar), which unfortunately did not fully restore stomach
absorption alongside a gradual process of repairing the lining of the
stomach and GI tract.
Note:
while adverse reactions from taking supplementary HCl are rare (e.g.,
I’ve never seen one), they do happen. Wright was thus adamant for these
precautions to be understood by anyone planning to attempt a HCl protocol
and strongly encouraged all patients to work with a physician familiar in
the protocols.
In
addition to taking HCl with each meal, it is also important to make sure
the supplement includes enzymes which digest proteins (particularly
pepsin—which almost always improved the clinical course of Wright’s
patients on HCl). Finally, since HCl requires chloride, chloride
supplementation (e.g., through unprocessed NaCl or KCl—celtic sea salt is
an excellent option) is often necessary as many Americans are on low
salts diets.
Finally,
since bitter foods increase stomach acid secretion, Wright often advised
consuming a bitter herb before a meal (keep in mind just tasting a bitter
is enough to induce stomach acid secretion). His preferred approach was
to drink a liquid preparation of gentian or artemisia—two of the most
commonly used herbal bitters preparations—five minutes before meals.
Beyond improving acid secretion, bitters also improve the rest of the
digestive process. For example in one German study which Wright cited
(but I could not find online):
The
researchers evaluated the effect of gentian root capsules in 205 people
with loss of appetite, heartburn, constipation, flatulence, abdominal
pain, nausea, and dyspepsia. They reported a rapid return of appetite and
dramatic relief of their GI symptoms.”
Finally,
sauerkraut (fermented cabbage), particularly if celtic sea salt is used
to produce it, is a strong simulator of stomach acid secretion and also
helps with digestion. As a result, many (like Dr. Mercola) recommend
drinking a few teaspoons of the juice from a sauerkraut ferment before a
meal.
Note:
Since PPIs are addictive, a variety of protocols exist for withdrawing
from them (functional medicine doctors often excel on this issue). While
some people can tolerate withdrawing from them cold turkey, many others
cannot. Generally speaking, the protocols for quitting them involve
reducing the PPI dose to the lowest you can tolerate, transitioning to a
less powerful antacid (e.g., a H2 blocker like Pepcid or Tagamet) and
then weaning off it.
Lowering Pressure on the LES
Numerous
approaches exist to reduce the pressure on the LES[iv].
Many of these in turn make sense if you think about them. Some of the
most common include:
•Sleep on an inclined bed. This
means raising the head of the bed by 4-8 inches (which people often have
to build up to), not sleeping on pillows so only part of
your body is elevated. One of the reasons why we experience so many of
the signs of silent reflux when we wake up is because lying horizontally
puts enough pressure on the LES while we sleep to cause small amounts of
acid reflux during the night—something we don’t similarly notice as we
stand vertically throughout the day.
•Avoid eating within three hours of bedtime
and avoid having heavy meals later in the day. They will often sit in the
stomach while you sleep and then
inevitably reflux out during the night.
•Try to avoid large meals where
you overstuff yourself.
•If
you sit or sleep so that there is a forward bend in your upper abdomen (which
is very common), this puts significant pressure on your stomach which
can result in reflux occurring. You need to sit straight (often we
instead are slightly curved forward) and lie vertically without too much
of an elevation in the top half of your body.
•Don’t
wear tight clothing that places a constrictive pressure on the abdomen
and thus the LES (this is also important for a variety of reason besides
preventing GERD).
•Try to avoid strenuous activities that increase inter-abdominal pressure
(e.g., bending from the waist, heavy coughing, workouts that involve
heavy lifting, and straining at the stool). Likewise, avoid exercising
immediately after eating.
•Consume
ginger (e.g., as a tea) because ginger accelerates gastric emptying
(thereby reducing pressure within the stomach).
•Consider
seeing a visceral body worker who can reduce the existing mechanical
strain on the stomach. Often hiatal hernias (which push the stomach
upwards into the diaphragm) can be manually reduced, and other forms of
tension which tug on the LES to open can be identified and treated with
appropriate body work. I have a few colleagues who specialize in this
work and they have all told me it is remarkably effective for GERD
(typically significantly improving it and often sufficing to treat it
completely without anything else being done).
Note: The most skilled person I know in this area shared that the
issue sometimes results from the peristaltic waves in the stomach being
abnormal and moving upwards through the stomach rather than downwards
into the duodenum or parts of the abdomen (e.g., the liver or the hole in
the diaphragm the esophagus travels though) pressing on the LES. Lastly,
they noticed that typically spicy foods tend to be the greatest issue for
individuals that have something directly tugging on the LES. I can’t
comment on their opinions, but given the success they’ve had, I felt it
was worth sharing.
•Be extra mindful of all of the above during pregnancy, since the
developing fetus puts additional pressure on the stomach.
Food Sensitivities
Earlier
this article I listed some of the most common foods which trigger GERD
(the most commonly cited are soda, caffeinated beverages like coffee,
alcohol, chocolate, spicy foods, tomatoes, mint and citrus). Patients
typically know which foods they are sensitive to (e.g., the previously
listed ones, milk, or lectin heavy foods like soy, cashews and quinoa),
but often cannot bring themselves to have the discipline to stop eating
them.
Note: in some cases, sensitivities to milk can be partially addressed
by also consuming lactase, an enzyme some are deficient in and which
breaks milk down in the GI tract.
So, if you work with someone who has reflux, it is important to identify
what their triggers are, and then encourage them to avoid those triggers.
If however the triggers are not known, it is typically advised to avoid
eating all of the foods commonly associated with GERD, and then add one
back in at a time until the GERD trigger is discovered.
Note: for children, either cow’s milk or infant formula is often a
trigger for reflux, which again is an argument for the critical importance
of breast feeding.
Furthermore,
in addition to irritating the stomach, food allergies (especially those
to milk), along with refined sugar, strong alcohol, and chlorine or
fluoride in the water can inhibit stomach acid production.
Finally,
while cigarettes are not technically a food, they are a common trigger
for reflux and smoking must often be stopped to treat reflux.
Repairing the GI Tract
Gastric
and duodenal ulcers are a frequent cause of pain and a fairly standard
protocol exists for treating them in medicine. Many people who wish to
avoid using pharmaceuticals are understandably reluctant to do the
conventional approach, but before you go down that road, I need to
emphasize that significant gastric bleeding (which can come from ulcers
and frequently are a complication of NSAID use) cause over 250,000
hospitalizations a year and around 20,000 deaths each year in the USA.
For this reason, if you suspect something is bleeding in your GI tract,
it is in your best interest to consult with a physician you trust.
Note: when bleeding occurs in the esophagus, stomach, or start of the
small intestine (where ulcers also develop), it will often cause you to
have black and tarry stools (as the blood is digested at this point). If
you have bright red stools (assuming it does not come from eating red
meat or beets), it comes from a bleed later in your GI tract such as an
anal fissure or a colon cancer.
The most commonly used treatment for healing ulcers and the inside of the
stomach is sucralfate,
an aluminum containing compound which forms a protective lining over the
stomach. Since it contains aluminum which then enters the body (e.g., it
can cause aluminum toxicity in patients with reduced renal function) I am
not the biggest fan of it. However, it does frequently help patients with
GI irritation or active ulcers and when used is typically combined with a
strong antacid while the GI damage is being healed.
One
of the most effective alternatives for treating GI tract damage is
licorice, particularly when its toxic component, glycyrrhizin, is removed
(known as deglycyrrhizinated licorice or DGL). DGL has repeatedly been
shown to treat gastric and duodenal ulcers, as effectively as many other
protocols (e.g., medications to suppress stomach acid). In addition DGL,
omega-3 fatty acids also can help with healing GI ulcers.
Note: DGL typically works best when tablets of it are chewed and then
swallowed with as little water as possible, since for it to work it needs
to have direct contact with the cells of the gastrointestinal lining
(likewise it works best when taken on an empty stomach).
In
addition to DGL, vitamin A, vitamin C, zinc, and especially L-glutamine
are known for helping to repair damaged GI tissue. Additionally slipperly
elm, aloe vera juice, chamomile (specifically for the esophagus), tumeric
and astaxanthin often
can help to protect GI tissue being irritated by stomach acid. Since the
responses to each of these varies, you may need to try a few before you
identify the one that works for you (or have someone you trust test which
one is appropriate).
H.Pylori
Helicobacter
pylori is a corkscrew shaped bacteria which lives in the stomach of about
half of the world’s population. It is commonly found within ulcers and a
variety of other GI tract pathologies, and in many cases has been
implicated as the causative agent for those issues. Furthermore, an
H.Pylori infection has also been shown to be strongly associated with
stomach cancer. Because of this, simple tests exist to
detect H. Pylori, and the bacteria is often a target in any attempt to
treat the stomach so extensive antibiotic regimens exist for eliminating
it.
Likewise,
since H. Pylori protects itself by eliminating stomach acid, integrative
practitioners have an additional reason to want to eliminate it as well.
Note: this may explain why lowering stomach acidity causes gastric
cancer, as once a more hospitable environment is created for H. Pylori,
it is more able to reproduce and cause stomach cancer.
A
variety of natural therapies in turn have been discovered which also
eliminate H.Pylori. These include:
•Mastic
Gum (this was Wright’s favorite option and also helped to treat GI
ulcers).
•Vitamin C (for those who have difficulty tolerating it, ascorbate rather
than ascorbic acid often solves the problem).
•Vitamin D (either consumed orally, or ideally gained through sunlight
exposure).
•Slipperly Elm (not as effective, but like vitamin C it also protects the
GI tract).
Note:
Given how common H. Pylori is (with half of humans having it), I have
often wondered if is as problematic as people make it out to be, or if it
actually serves a vital role and only becomes problematic when the body
is out of balance (e.g., due to the wrong diet or too little stomach
acid). Since H. Pylori affects both stomach acidity and a variety of gut
hormones, it is possible the bacteria has an important regulatory
function as well.
Conclusion
Despite
everything I’ve come to understand about the politics of medicine, I still have difficulty believing medical
science does not acknowledge the importance of stomach acid.
Situations like this hence become some of the clearest illustration that modern
medicine is much more a sales directed business than a science.
Fortunately however, since the PPI patents are finally expiring (which
means it is no longer highly profitable to sell the drugs) there at last
is no longer an incentive to keep on ignoring the harms of these
medications and medical science is at last “discovering” the harms of
these drugs.
I
hope that this article was helpful to each of you, and I sincerely thank
you from the bottom of my heart for both taking the time to read it and
to share it with those who can benefit from it.
This post is public so feel free to
share it.
Share
Invite your friends and earn rewards
If you enjoy The
Forgotten Side of Medicine, share it with your friends and earn rewards
when they subscribe.
Invite Friends
© 2023 A
Midwestern Doctor
Substack Inc., 111 Sutter St 7th Floor, San Francisco, United States
94104
Unsubscribe
|
 Note:
the population vaccination percentages were sourced from
Note:
the population vaccination percentages were sourced from